365
Views & Citations10
Likes & Shares
CASE
A 31-year-old primigravida at 37 weeks of gestation with gestational diabetes mellitus on insulin was hospitalized with the complaints of fever and cold for 1 day. She tested positive for COVID-19. This pregnancy was spontaneous conception and she received antenatal care in private hospital. Her first and second trimesters were unremarkable. There were no contributing factors from her past medical, surgical and familial history. Routine antenatal investigations including virological markers were normal. Her first and second trimester USG reports were normal. Her USG at 30 weeks reported posterior low-lying placenta the lowermost edge of which was 4 cms from internal Os. She was diagnosed as gestational diabetes (GDM) at 32 weeks of pregnancy and was on insulin and medical nutrition therapy. During admission her sugar profile was normal, and she was not dyspneic. Hence, she was conservatively managed for COVID -19 infection. Her USG at 37 weeks reported posterior low-lying placenta with a fetal weight of 2.7 kg and adequate liquor. She underwent induction of labor at 38 weeks of gestation for GDMA2. Cervical ripening was done with foley catheter followed by sublingual misoprostol.
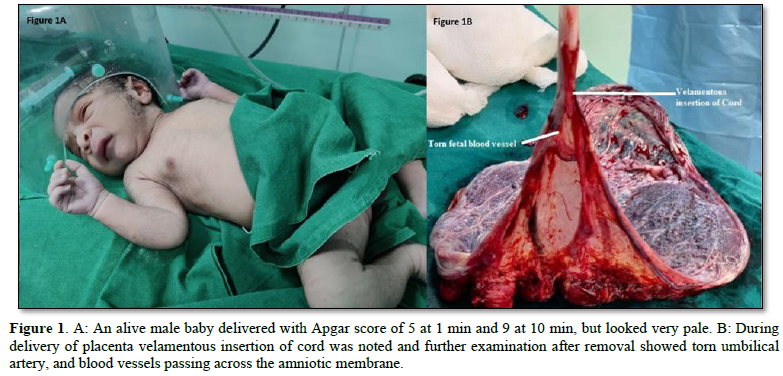
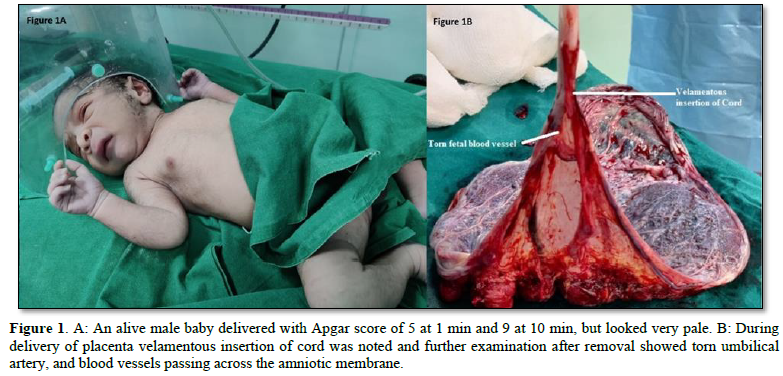
Low dose Oxytocin protocol was initiated following misoprostol when her cervix was 50% effaced, 2cm dilatation and station at -3 cms. Artificial rupture of membrane (ARM) was performed after 4 h of oxytocin at 5cm of cervical dilation vertex station at -3cms and liquor was clear. Immediately following ARM fetal heart rate was normal but after 10 min of post procedure, fetal heart rate started decelerating up to 60 bpm which did not pick up measures of intrauterine resuscitation. She started having fresh bleeding per vaginum and passed a clot of 30-50 gms and per vaginal examination was repeated and cervix was 5 cm dilated, vertex at 0 station. Hence was taken up for emergency LSCS under GA in view of persistent fetal bradycardia due to suspicion of abruptio placentae. Intraoperatively umbilical cord was present below the presenting part, liquor was clear and there was no evidence of abruption. An alive male baby delivered with Apgar score of 5 at 1 min and 9 at 10 min, but looked very pale (Figure 1A). There was no postpartum hemorrhage. During delivery of placenta velamentous insertion of cord was noted and further examination after removal showed torn umbilical artery, and blood vessels passing across the amniotic membrane (Figure 1B). Baby was pale and hemoglobin was 12 gm %. On 4th day of post LSCS, the mother and baby were discharged.
DISCUSSION
Vasa previa is an abnormal condition in which fetal vessels are unsupported in the amniotic membrane and run across the lower segment of the uterus just above the internal Os. They are predisposed to rupture when amniotic membranes rupture and cause fetal exsanguination resulting in still birth or birth of deeply asphyxiated fetus. Fetal mortality is reported to range from 22-100% [2]. This condition was recognized in pre-Ultrasound era by the triad of rupture of membranes, painless vaginal bleeding and fetal distress or fetal death. In the current era usually, the diagnosis is possible during antenatal period as early as second trimester by USG [3]. But still 10-16 % of cases are missed in spite of undergoing USG as it happened in this lady [4]. Dutta and colleagues reported a similar case where APH with fetal distress was diagnosed due to fresh bleeding per vaginum after spontaneous rupture of membranes in labor. Delivery was carried out by emergency LSCS and the baby looked pale and the placental examination showed velamentous insertion of cord with rupture of vessel [5]. The neonate’s hemoglobin was 12 gm % and did not require transfusion and this is because the delivery could be affected within 15 min of onset of bleeding. Jantarasaengaram [6] and colleagues reported a similar case at 34 weeks of pregnancy which was referred to them as APH and USG showed low lying placenta with suspicion of vasa previa and NST revealed decreased FHR variability with normal FHR. The fetus was delivered by emergency LSCS and the neonate required blood transfusion. Placental examination after delivery revealed velamentous insertion of cord with rupture of vein [6]. In the current case also, Vasa previa could be diagnosed after Caesarean delivery for suspected abruption.
The emergency of the condition has profound effect on the mental status of women and a study which explored women’s perception when diagnosed with vas previa revealed feelings of uncertainty of the fetal outcomes, stress, considering it as inconsistent and inadequate information during labor and feeling like time-bomb when diagnosed antenatally [7]. Antenatal diagnosis of velamentous insertion of cord and vasa previa can be done with 2D scan combined with color Doppler and Pulsed Doppler. On 2D scan the vessels appear as immobile linear structures close to uterine wall and on color Doppler the separation of vessels in the amniotic membrane away from placental edge can be visualize. With the help of Power Doppler, the vessels can be differentiated whether they are of maternal or fetal origin [8]. Guidelines are in place for diagnosis and management of Vasa previa. The SOGC guidelines state that when placenta was found to be low-lying on routine second trimester scan further evaluation to be carried out to see cord insertion site. Transvaginal USG with Color Doppler to be undertaken for all women with risk factors for vasa previa and diagnosis is possible with combination of Transvaginal and transabdominal USG. Women with antenatally diagnosed Vasa previa are to be delivered by Caesarean section before the onset of labor for good fetal outcomes [9]. Recent Greentop guidelines also confirm that USG accuracy in diagnosing Vasa previa is high and caesarean delivery should occur between 32-34 weeks after administration of corticosteroids for fetal lung maturity [10]. The neonatal survival rates were reported to be 97% and 44% respectively for those diagnosed antenatally and not diagnosed antenatally and the neonatal blood transfusion rates were high 58.4% for those not diagnosed antenatally [11]. Vasa previa when suspected clinically after rupture of membranes (spontaneous or artificial) needs urgent delivery foregoing confirmation by USG as the amount of blood lost may appear small but may be fatal as fetal blood volume is 80-100ml/kg at term [10].
The risk factors for vasa previa identified were bilobed and succenturiate placentas, low-lying placentas Multiple pregnancies resulting from IVF Marginal insertion of the cord Velamentous insertion of the cord Palpable vessel or a suspected amniotic band is felt on vaginal exam. A high index of suspicion for vasa previa is required before amniotomy as missing the diagnosis is common [12]. Cases are under reported the prevalence ranges from 1in 200 to 1in 5000 pregnancies [10] and the meta-analysis repots 0.46 cases per 100 deliveries [13]. Vasa previa is also known as Benckiser’s hemorrhage and it should be suspected during labor with onset of dark bleeding following rupture of membranes.
CONCLUSION
It is easy to miss Vasa previa by 2D-USG. Risk factors for vasa previa are well defined and every effort should be made to rule out Vasa previa especially in low lying placentas as in this case. Decision to delivery interval is important to avoid still birth or severe fetal asphyxia.
- Oyelese Y, Catanzarite V, Prefumo F, Lashley S, Schachter M, et al. (2004) Vasa previa: The impact of prenatal diagnosis on outcomes. Obstet Gynecol 103(5): 937-942.
- Fung TY, Lau TK (1998) Poor perinatal outcome associated with vasa previa: is it preventable? A report of three cases and review of the literature. Ultrasound Obstet Gynecol 12(6): 430-433.
- Derbala Y, Grochal F, Jeanty P (2001) Vasa previa. J Prenat Med 1(1): 2-13.
- Catanzarite V, Maida C, Thomas W, Mendoza A, Stanco L, et al. (2001) Prenatal sonographic diagnosis of vasa previa: Ultrasound findings and obstetric outcome in ten cases. Ultrasound Obstet Gynecol 18(2): 109-115.
- Datta S, Babu KM, Mitra S, Patil D (2007) Vasa previa: An avoidable obstetric tragedy. J Obstet Gynaecol India 66(3): 185-187.
- Jantarasaengaram S, Suthipintawong C, Kanchanawat S, Thanagumtorn K (2007) Ruptured vasa previa in velamentous cord insertion placenta. J Perinatol 27(7): 457-459.
- Javid N, Sullivan EA, Halliday LE, Duncombe G, Homer CS (2014) Wrapping myself in cotton wool: Australian women's experience of being diagnosed with vasa previa. BMC Pregnancy Childbirth 14(1): 318.
- Gandhi A (2020) Atypical vasa previa in a velamentous cord insertion identified during sonographic examination. J Diagn Med Sonogr 36(1): 73-78.
- Gagnon R, Morin L, Bly S, Butt K, Cargill YM, et al. (2009) Guidelines for the management of vasa previa. J Obstet Gynaecol Can 31(8): 748-753.
- Jauniaux ER, Alfirevic Z, Bhide A, Burton G, Collins S, et al. (2018) Vasa previa: Diagnosis and management. Green‐top guideline No. 27b. BJOG Int J Obstet Gynaecol 126(1): e1-e48.
- Gagnon R (2017) No. 231-Guidelines for the Management of vasa previa. J Obstet Gynaecol Can 39(10): e415-e421.
- Lijoi AF, Brady J (2003) Vasa previa diagnosis and management. J Am Board Fam Pract 16(6): 543-548.
- Pavalagantharajah S, Villani LA, D’Souza R (2020) Vasa previa and associated risk factors: A systematic review and meta-analysis. Am J Obstet Gynecol MFM 2(3): 100117.
QUICK LINKS
- SUBMIT MANUSCRIPT
- RECOMMEND THE JOURNAL
-
SUBSCRIBE FOR ALERTS
RELATED JOURNALS
- Journal of Infectious Diseases and Research (ISSN: 2688-6537)
- Journal of Ageing and Restorative Medicine (ISSN:2637-7403)
- Journal of Cancer Science and Treatment (ISSN:2641-7472)
- Journal of Nursing and Occupational Health (ISSN: 2640-0845)
- Journal of Otolaryngology and Neurotology Research(ISSN:2641-6956)
- Advance Research on Alzheimers and Parkinsons Disease
- International Journal of Diabetes (ISSN: 2644-3031)